Carotid arteries are located on either side of your neck. It provides oxygen, nutrients, and blood to the brain. The oxygenated blood towards the head is supplied through your carotid arteries and vessels. The carotid artery supplies oxygenated blood and nutrients; the brain performs function properly. It is situated on both sides of your neck.
Learning that your carotid artery blocks can be stressful, especially after a stroke. Questioning how long someone might expect to live with a blocked carotid artery is typical, especially if it is recently diagnosed. To explore how blocked carotid artery might develop. What is the life expectancy with blocked carotid artery and its treatment-related surgical techniques? This blog will help you.
What are the Causes of the blocked carotid artery:
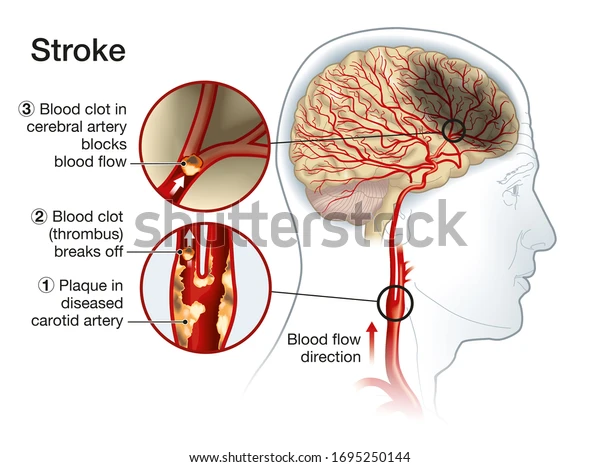
The leading cause of artery blockage is atherosclerosis. It includes plaque formation in the carotid, which creates resistance in blood flow or oxygen toward the brain. The plaque may be of cholesterol, lipids, or calcium. Basically, atherosclerosis increases the risk of stroke and arterial damage. As the severity of the carotid blockage, the more chances of stroke
In the condition of stroke, due to blockage of carotid artery, cuts off the supply towards the brain. As a result of this. Brain cells don’t get oxygen and begin to die. It is fatal and causes mental and physical impairment. Some reasons for blockage are given below:
- Genetics
- High blood pressure
- Hyperlipidemia
- Diabetes
- Injury to your neck, old age
- Smoking or using alcohol.
People with two or more of these risk factors face an elevated risk of stroke and may need aggressive treatment to reduce their chances of death1
Life expectancy with blocked carotid artery with symptoms:
However, in many cases, the patient doesn’t experience symptoms or is asymptomatic. However, the patient suffering carotid artery blockage may experience a heart attack or stroke called a silent attack.
Symptoms depend on the severity of the blockage; different patients experience different symptoms;
- Memory loss
- Confusion
- numbness in one body side
- Fainting due to loss of blood supply to the brain
- Memory, speech, and thinking problems
A recent international study indicates that timely treatment of blocked carotid arteries, including surgical interventions like carotid endarterectomy or minimally invasive procedures like angioplasty and stenting, can significantly improve long-term survival rates. In some cases, these treatments have been shown to extend life expectancy by over 10 years.2
Life expectancy with blocked carotid artery treatment:
To reduce your risk of having another stroke, your doctor can advise an invasive surgical surgery if they find that your carotid arteries are blocked. When carotid artery blockage exceeds 70%, doctors may recommend surgical intervention, such as carotid endarterectomy or carotid stenting, to reduce the risk of stroke. The decision to proceed with surgery depends on several factors, including whether the patient is symptomatic, their overall health, and the presence of other risk factors. In cases where the blockage is less severe (below 70%), doctors often prioritize non-surgical treatments, such as medication and lifestyle changes, to manage the condition. Although below 70 per cent obstruction, doctors treated with medicines.
Whereas, What is the life expectancy with 100 blocked carotid artery? It becomes serious and life-threatening. Further, timely diagnosis of blockage may lead to long productive lives. Along with these, other health parameters also define its life expectancy. However, there is no well-defined set of time for an individual’s life with artery blockage.
Clinical Guidelines for Carotid Artery Blockage Treatment:
For Symptomatic patients:
These patients show clinical signs of carotid artery disease, such as stroke or transient ischemic attack (TIA). For symptomatic patients with carotid artery stenosis of 70% or more, surgery is generally recommended.
The most common surgical options are carotid endarterectomy (CEA) and carotid stenting. Surgery is intended to reduce the risk of a future stroke, as these patients have a higher risk of stroke due to the blockage.
For Asymptomatic patients:
These individuals do not exhibit any signs of stroke or TIA. For asymptomatic patients with 70% or more blockage, the decision for surgery is more nuanced. Factors such as age, overall health, and the presence of other cardiovascular risk factors (e.g., diabetes, hypertension) are considered. While surgery may still be recommended in high-risk patients, many asymptomatic patients with severe blockage can initially be managed with medications, lifestyle changes, and close monitoring. The benefits of surgery must outweigh the surgical risks.
Treatment Options Based on Blockage Severity:
Mild to Moderate Blockage (50%-69%):
For patients with blockage in this range, especially if asymptomatic, treatment typically focuses on medication (e.g., statins) and lifestyle adjustments (e.g., smoking cessation, dietary changes). Surgical intervention is usually not considered unless there are other complicating factors, such as the presence of symptoms or significant risk factors for stroke.
Severe Blockage (70%-99%):
When the blockage exceeds 70%, surgery is often considered for both symptomatic and asymptomatic patients, although the decision is based on individual risk factors. Carotid endarterectomy is the most widely used surgical procedure and is associated with a reduced risk of stroke in patients with significant stenosis. Carotid stenting may also be recommended, particularly for patients who are not good candidates for surgery due to other health conditions (e.g., high surgical risk or anatomical challenges).
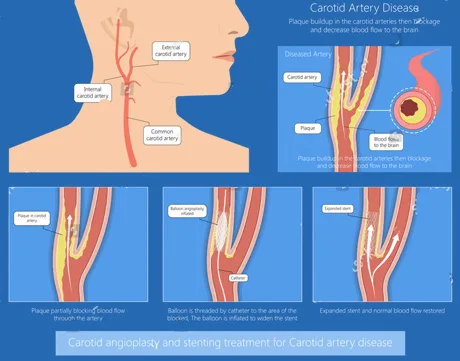
Carotid artery angioplasty with stenting:
The stent placement inside your carotid artery is one of these procedures. A constricted blood artery is kept open with the help of a portion of a thin mesh tube to maintain proper blood flow. But, even while it may sound frightening, the blockage hazards remain there. However, cholesterol and diabetes-controlling medicines, in addition to antiplatelet also used along with this treatment.
Stenting is also often considered for older patients or those with comorbidities that make surgery more risky. However, stenting is associated with a slightly higher risk of complications, such as stroke or vascular injury, during the procedure.
Carotid endarterectomy(CEA):
Carotid endarterectomy is another technique (CEA.) In this kind of surgery, the affected artery is clamped before the obstruction is taken out and removed. Following the excision, the blocked artery can be patched using a vein segment from your leg. The artery and neck are then repaired using stitches.
CEA typically preferred for younger patients, those with good overall health, or those who have an anatomy that makes stenting difficult (e.g., tortuous arteries).
Doctors generally regard the carotid endarterectomy CEA process as safe. It significantly lowers the risk of stroke in people with carotid artery blockages. Several studies have demonstrated a significantly reduced risk of stroke on the afflicted side following a CEA. Thus, it’s a process that tangibly lengthens their expected lifespan.
The International Carotid Stenting Study (ICSS), led by researchers at University College London, compared the effectiveness of carotid endarterectomy and carotid stenting in reducing the risk of stroke and death. The study found that both procedures significantly lower the likelihood of fatal stroke in patients with severe carotid artery stenosis. While each treatment has its own risks and benefits, these findings support the use of endarterectomy or stenting as effective options for reducing stroke-related mortality in carefully selected patients3.
Other Health Factors in Treatment Decisions:
Age and General Health:
Younger, healthier patients are generally better candidates for carotid endarterectomy, as they can tolerate surgery and benefit from the long-term protection against stroke. In contrast, older patients or those with multiple health conditions, such as heart disease or diabetes, may benefit more from stenting as a less invasive option.
Risk Factors:
Patients with high blood pressure, diabetes, high cholesterol, or a history of smoking may be at higher risk for complications from surgery or stenting. These factors can influence both the treatment choice and the long-term management plan. For example, patients with poorly controlled diabetes might be more prone to complications, making stenting a preferred option in some cases.
Follow-up Care and Monitoring:
After surgical treatment (whether endarterectomy or stenting), patients need regular follow-up care to monitor the patency of the artery, detect any recurrence of plaque buildup, and manage cardiovascular risk factors.
Lifestyle changes, such as diet, exercise, and medication adherence, are crucial in preventing the reoccurrence of carotid artery disease.
Potential Risks and Benefits of Stenting and CEA Surgery:
Risks and Benefits related to Carotid Artery Stenting (CAS):
Benefits:
- Less Invasive: Typically performed through a small incision in the groin.
- Shorter Hospital Stay: Recovery time is often shorter compared to CEA.
- Lower Risk of Nerve Damage: Reduced risk of damage to nerves in the neck.
Risks:
- Stroke: There’s a risk of stroke, particularly during the procedure.
- Bleeding: Potential for bleeding at the insertion site.
- Allergic Reaction: Risk of allergic reaction to contrast dye used during the procedure.
- Kidney Damage: Contrast dye can sometimes damage the kidneys.
- Stent Failure: The stent may become blocked or dislodge.
Risks and Benefits related to Carotid Endarterectomy (CEA):
Benefits:
- Effective Plaque Removal: Directly removes plaque from the artery.
- Long-Term Results: Often provides long-lasting relief.
Risks:
- Stroke: There’s a risk of stroke, particularly during the procedure.
- Bleeding: Potential for bleeding from the incision site.
- Nerve Damage: Risk of damage to nerves in the neck.
- Infection: Risk of infection at the incision site.
It’s important to note that the specific risks and benefits of each procedure can vary depending on individual factors such as overall health, the severity of the blockage, and the skill of the surgeon.
Frequently Ask A question:
What is the average carotid artery blockage by age?
With time carotid artery blockage becomes worse gradually. At the age of 40, most men suffer from plaque of cholesterol. This worsens with the passage of age; many plaques have built up. Although blocked carotid artery by age also depends upon different other factors such as diet, lifestyle, chronic diseases such as diabetes, blood pressure etc.
What are the symptoms of a blocked artery in your neck?
The symptoms include:
- Pain in the neck or tenderness
- difficulty in swallowing and speaking
- visual changes occur
- Reduce pulse in the neck
Besides these, other symptoms include:
- headache
- numbness
- Reduce blood flow in one side of the body. It might be due to transient ischemic attack.
- confusion or loss of memory
Life expectancy with blocked carotid artery without surgery?
It depends on the blockage area. If the area is above 70 per cent. Surgery is an option. In less blockage areas, medication, lifestyle changes and diet plans are prescribed. However, if the condition gets worse then less invasive surgery such as stenting or balloon angioplasty surgery should be carried out.
Conclusion:
Living a healthy lifestyle coupled with a healthy diet is essential to extend your life expectancy with blocked carotid artery. It also increases your quality of life. If you are a diabetic, emphasize on such foods that reduce sugar level. Your life expectancy chances increase considerably if you stop smoking, consume a nutritious diet, exercise frequently, and take your medications as directed in blocked carotid artery conditions. Whether you’ve recently been diagnosed with a stroke or already suffer from one, it is true. Also, following up with your doctor is crucial to monitor your condition.

Leave a Reply